Master ABA CPT Codes 97153-97158: Avoid Costly Audit Findings in 2025
Navigating ABA therapy CPT codes 97153–97158 correctly is essential for compliant billing and avoiding costly audit findings. With major regulatory changes implemented throughout 2025, understanding these codes' specific requirements can save your practice thousands in denied claims and compliance issues.
Here's the thing—the billing landscape changed dramatically this year. New telehealth codes replaced old phone consultation codes, and documentation requirements got stricter than ever.
Understanding the Core ABA Therapy CPT Codes
CPT Code 97153: Technician-Led Individual Therapy
CPT Code 97153 covers one-on-one adaptive behavior treatment delivered by a behavior technician (RBT) under BCBA supervision. This code applies when technicians follow established protocols without making real-time modifications.
But here's what's crucial: you can't just implement any behavior plan. The ABA CPT code updates for 2025 emphasize that proper technician qualifications must be documented for every claim.
When to Use 97153:
- RBT follows established treatment protocols
- No immediate protocol changes are made during session
- Direct 1:1 client interaction with skill-building focus
- Routine data collection and program implementation
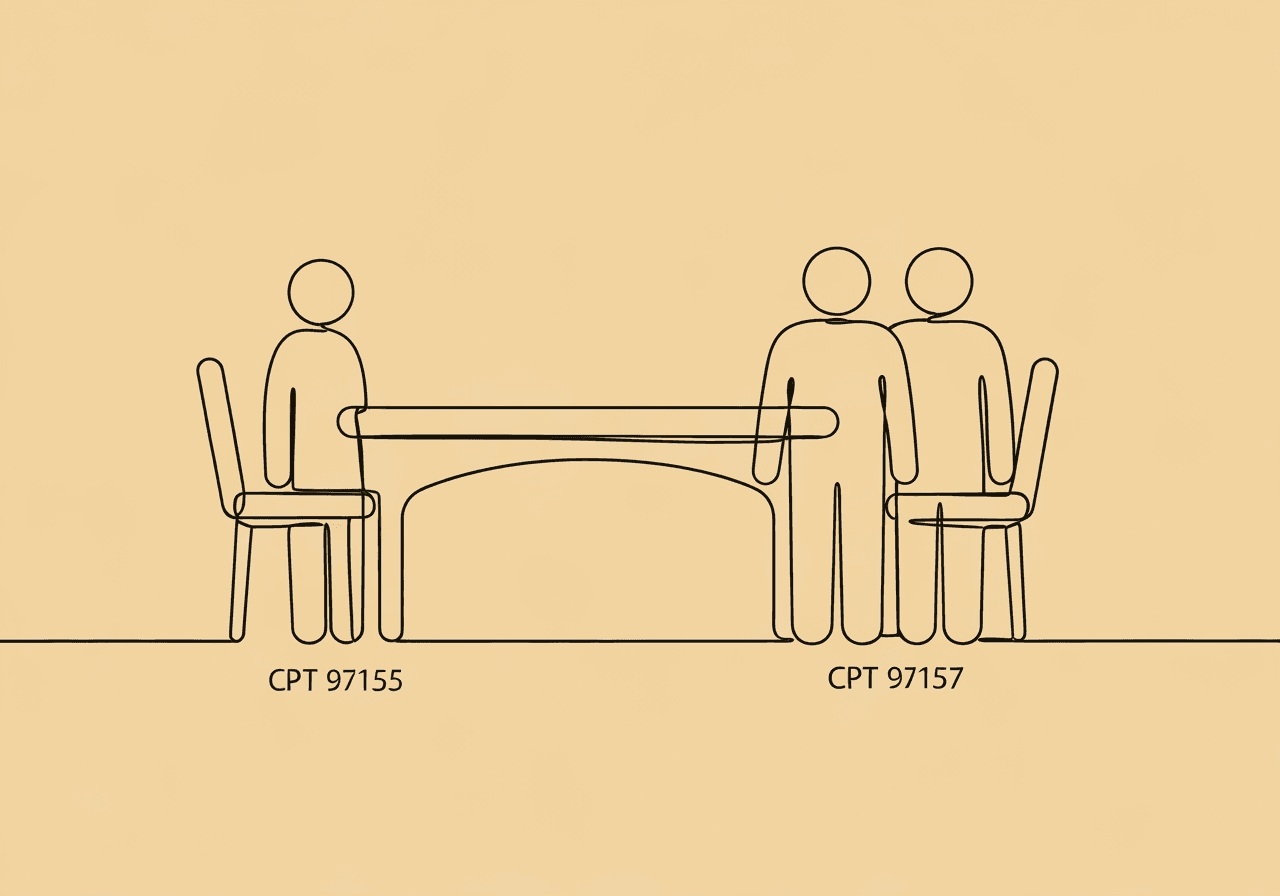
CPT Code 97155: BCBA-Led Protocol Modification Services
CPT Code 97155 represents direct service by a qualified health professional (BCBA) who actively modifies treatment plans based on real-time client responses. This isn't for passive supervision—it requires hands-on clinical decision-making.
The complete guide to ABA therapy CPT codes makes one thing clear: BCBAs must demonstrate direct involvement in treatment modifications, not just oversight.
When to Use 97155:
- BCBA directly engaged with client or directing technician
- Real-time treatment adjustments based on client response
- Active protocol modification with clinical justification
- Not for passive supervision or data review
Group and Family Therapy Codes
CPT Code 97154 covers group treatment led by a behavior technician under supervision, allowing cost-effective service delivery to multiple clients simultaneously.
CPT Code 97158 represents group treatment sessions led by a qualified health professional without requiring protocol modification.
CPT Codes 97156 and 97157 specifically address family therapy and caregiver training services. Family involvement has proven critical for treatment success.
Critical Documentation Requirements
For CPT Code 97155 Documentation
Proper CPT code 97155 documentation must include:
- Session duration in 15-minute increments
- Specific treatment modifications with clinical rationale
- Client response to protocol changes
- Objective data supporting modifications
- Future treatment plan adjustments
Common Documentation Errors to Avoid
Documentation mistakes that trigger audit attention include:
- Failing to document protocol modifications when billing 97155
- Not specifying BCBA's direct involvement in treatment
- Using 97155 for routine protocol implementation
- Billing 97155 for indirect work like data review outside sessions
Want to avoid these pitfalls? Each note needs to tell the story of clinical decision-making, not just record activities.
Audit-Proof ABA Billing Practices
Service Distinction Requirements
97155 should only be reported when the BCBA is either directly engaged with the patient or directing a technician in implementing modified protocols. The official ABA billing guidelines are crystal clear: treatment planning conducted independently while technicians work with patients doesn't qualify for 97155 billing.
Concurrent Billing Compliance
You can bill 97155 and 97153 concurrently as they represent separate services, but documentation must support the distinct nature of each service provided. Think of it this way—if someone audits your file, they should immediately understand why both codes were necessary.
Credentialing Impact
Uncredentialed providers cannot generate reimbursable services regardless of code accuracy. Always verify provider credentials match payer requirements before service delivery.
2025 Regulatory Changes and Billing Updates
Major CPT Code Changes
The American Medical Association made significant updates in 2025, with 270 new codes added and 112 outdated codes removed. Most importantly for ABA providers:
- Traditional telephone E/M codes (99441-99443) were deleted
- Seventeen new synchronous telemedicine codes (98000-98015) were added
- Digital therapeutic intervention codes (98975-98978) were revised
Reimbursement Rate Updates
Starting May 1, 2025, new maximum allowed amounts took effect for primary ABA billing codes including 97151, 97153, 97155, and 97156.
New Authorization Requirements
Beginning October 15, 2025, providers must submit service authorizations that include specific units requested for each ABA CPT code used for treatment. This represents a major shift from previous practices.
Insurance Billing Best Practices
Preauthorization Requirements
Some payers require specific prior approval for CPT code 97155. Always verify authorization requirements to avoid claim denials and potential audit findings.
Common Billing Errors
Frequent mistakes that trigger payer scrutiny:
- Incorrect session duration documentation
- Inadequate treatment plan documentation
- Services by uncredentialed providers
- Using deleted telephone codes instead of new telemedicine codes
Quality Assurance Protocols
Implement regular reviews of 97155 usage to ensure protocol modifications are clinically appropriate and properly documented. This prevents upcoding practices that present significant compliance risks.
Plus, about 30% of new codes are Category III codes for emerging technology—make sure you're billing the right ones.
Federal Oversight Landscape
Increased Audit Activity
The Office of Inspector General has intensified focus on ABA billing patterns, particularly examining questionable usage of higher-level codes like 97155 without proper documentation.
State-Specific Requirements
ABA billing codes 2025 requirements vary significantly by state, making attention to state-specific billing rules and documentation standards crucial for compliance. Virginia's recent authorization changes are just one example of how quickly regulations evolve.
Frequently Asked Questions
Can RBTs bill under CPT code 97155?
No, only BCBAs or licensed behavior analysts can provide services under CPT code 97155. RBTs typically bill under 97153 for direct therapy services.
What's the difference between 97153 and 97155?
97153 is for routine protocol implementation by technicians, while 97155 requires real-time protocol modifications by qualified professionals during direct client interaction.
Can I still use telephone codes for ABA services?
No, traditional telephone E/M codes (99441-99443) were deleted in 2025. You must use the new synchronous telemedicine codes (98000-98015) for virtual services.
How detailed should my 97155 documentation be?
Documentation must specifically describe protocol modifications made, rationale for changes, client response, and impact on future treatment planning. Generic notes won't survive an audit.
What triggers an ABA billing audit?
Common triggers include unusual billing patterns, high 97155 usage without justification, credentialing discrepancies, and inadequate documentation supporting medical necessity.
Do I need separate authorizations for each CPT code now?
Starting October 15, 2025, yes—service authorizations must include specific units requested for each ABA CPT code used for treatment.
Staying compliant with audit-proof ABA billing requires ongoing attention to documentation quality, proper code selection, and awareness of rapidly changing regulations. By understanding these requirements and implementing robust quality assurance practices, you can ensure your billing practices withstand regulatory scrutiny while maintaining access to essential ABA services.
Ready to streamline your documentation process and stay ahead of 2025's billing requirements? Create compliant ABA session notes that meet today's strict documentation standards with our HIPAA-aligned platform.
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,5448 min read - 2
CPT Code 97153: Complete Guide for RBTs
3,9979 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
2,9709 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,4764 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,7127 min read
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,5448 min read - 2
CPT Code 97153: Complete Guide for RBTs
3,9979 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
2,9709 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,4764 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,7127 min read
Related Resources
Explore more helpful content on similar topics
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
Learn how CPT code 97153 ABA ensures accurate billing and compliance in 2025. Discover key documentation tips and insurance ABA billing strategies.
CPT 97155 vs 97157: Documentation Guide for BCBAs
Master CPT 97155 vs 97157 documentation for BCBAs. Discover key differences in service definitions, required elements, ethical tips, and scenarios for group adaptive behavior treatment and protocol modifications to ensure compliance.
1:1 RBT Staffing Documentation: Clinical Guide
Struggling with 1:1 RBT staffing documentation? Discover clinical criteria for necessity, data-driven justification strategies, and essential docs to help BCBAs avoid audits, secure funding, and maintain ethical ABA practices.