Autism Aggression ABA: Complete 2025 Guide to Assessment & Intervention

Managing Autism Aggression ABA: A Comprehensive Clinical Guide for BCBAs and RBTs
If you've worked in ABA for more than a few months, you've likely encountered it—that moment when a client's frustration boils over into physical aggression. Maybe it's a 12-year-old hitting peers during transitions, or a teenager throwing materials when asked to complete a non-preferred task. These situations test every skill we have as practitioners.
Autism aggression ABA interventions demand our most sophisticated clinical thinking, evidence-based strategies, and rock-solid safety protocols. The reality is sobering: research shows that 32.8% to 68% of individuals with autism spectrum disorder experience aggressive behaviors, making this the most critical challenge many of us will face in practice.
What makes aggression so complex? It's not just about stopping the behavior—we're working to understand why it's happening, keep everyone safe, teach better ways to communicate needs, and document everything meticulously for families, schools, and insurance providers.
This guide walks you through the clinical tools, safety protocols, and documentation frameworks you need to address aggressive behavior effectively while staying compliant with rapidly evolving regulatory standards.
Defining Aggression in Applied Behavior Analysis
Here's where precision becomes everything. Aggression in ABA refers to any behavior directed toward another person that has the potential to cause harm or discomfort. This includes physical acts like hitting, biting, kicking, pinching, or scratching, plus behaviors directed at objects that could endanger others—think throwing chairs or property destruction near people.
But here's what I've learned after years of practice: generic definitions don't help anyone. You need operational definitions so specific that any team member could identify the behavior immediately. Instead of writing "Client is aggressive," document exactly what you're seeing: "Client strikes others with closed fist making contact above the shoulders" or "Client throws materials with force exceeding 3 feet from their location."
Why does this matter so much? Because these precise definitions become the foundation for everything else—data collection, intervention planning, and those crucial conversations with insurance companies about medical necessity.
Common Functions of Aggressive Behavior
Understanding why aggression happens changes how we respond to it. Research consistently identifies four primary functions, and recognizing these patterns can transform your intervention approach.
Attention-seeking aggression occurs when clients have learned that aggressive acts reliably produce caregiver or peer attention—even negative attention. I've seen kids who receive more adult interaction in the 10 minutes after hitting someone than they got all morning during appropriate behavior. That's powerful reinforcement, even if it includes redirection and consequences.
Escape or avoidance functions drive aggression when clients use these behaviors to get out of demanding situations. Think about it from their perspective: if hitting staff consistently results in being removed from math worksheets, that behavior makes perfect sense. We've inadvertently taught them an effective (though problematic) coping strategy.
Tangible-seeking aggression emerges when clients access preferred items, activities, or locations through aggressive behavior. A client who obtains their preferred tablet by hitting staff has established a clear functional relationship. The aggression works—until we change the contingencies.
Automatic or sensory functions involve aggression that produces internal stimulation or serves self-regulation purposes. Some clients engage in head-banging or self-injury to manage sensory overload or achieve desired sensory input. These behaviors often look different from socially-mediated aggression and require different intervention approaches.
Here's what experience teaches: many aggressive behaviors serve multiple functions simultaneously, and these functions can shift over time as environmental conditions change.
Risk Screening and Safety Prioritization Workflow
Safety planning starts before you ever meet the client. Risk screening isn't just paperwork—it's your roadmap for keeping everyone protected while building therapeutic relationships.
Initial Risk Assessment Protocol
Every new client requires comprehensive risk screening that goes beyond reviewing previous incident reports. You're looking for patterns and environmental factors that increase risk.
Historical patterns tell a story. Examine frequency, intensity, duration, and circumstances surrounding previous incidents. But don't just read—talk to previous providers, teachers, and family members. They often share crucial details that don't make it into formal reports.
Physical capabilities matter enormously. A 40-pound child and a 150-pound teenager require completely different safety considerations, even with identical behavioral topographies. Consider not just size but also cognitive abilities, communication skills, and previous learning about behavioral consequences.
Environmental risk factors include access to potential weapons, confined spaces, or situations that historically trigger aggression. I've learned to walk through environments with fresh eyes, imagining how spaces might look to someone in crisis. That decorative vase becomes a projectile; that narrow hallway becomes a bottleneck during evacuations.
Communication abilities and current coping strategies reveal crucial information about intervention possibilities. Clients with limited communication often rely more heavily on aggression because it's their most effective way to influence their environment.
Safety Prioritization Decision Tree
When multiple challenging behaviors coexist (and they usually do), prioritize using this hierarchy:
- Immediate danger to self or others - Address life-threatening behaviors first, no exceptions
- Moderate physical harm potential - Target behaviors causing injury or property damage
- Interference with learning - Address behaviors preventing skill acquisition
- Social impact - Consider behaviors affecting relationships and community access
This systematic approach ensures your energy goes to the most critical safety concerns while building toward comprehensive behavior support. Plus, insurance companies want to see this kind of clinical reasoning in your documentation.
Assessment Toolkit for Severe Aggression
Comprehensive assessment combines multiple methods to build a complete picture of what's driving aggressive behavior. Here's how to approach it systematically.
Indirect Assessment Measures
Functional Assessment Screening Tool (FAST) provides rapid screening for potential behavioral functions through caregiver interviews. This 16-item checklist helps you identify likely maintaining variables before investing in more intensive assessment procedures. It's not definitive, but it points you in the right direction.
Questions About Behavioral Function (QABF) offers more comprehensive screening, examining attention, escape, nonsocial, physical, and tangible functions through detailed caregiver ratings. The beauty of the QABF is how it captures subtle patterns that might not be obvious during brief observations.
Remember: these tools never stand alone. They provide essential background information that guides your next assessment steps while identifying potential safety concerns you might have missed.
Descriptive ABC Analysis
Antecedent-Behavior-Consequence (ABC) data collection involves systematic observation of naturally occurring aggressive episodes. This is where you become a behavioral detective, looking for patterns in environmental triggers and maintaining consequences.
Effective ABC data requires specific descriptions that actually help with intervention planning. "During transition from preferred activity to non-preferred task with 3 peers present in classroom with typical noise level" tells you infinitely more than "during group time."
Precise behavior documentation using your operational definitions is crucial. Record duration, intensity, and specific topography of each aggressive episode. If someone else reads your ABC data, they should be able to picture exactly what happened.
Comprehensive consequence tracking includes everything that happens after aggression—natural environmental responses, planned interventions, peer reactions, and environmental changes. Often the maintaining consequences aren't obvious at first glance.
Here's a practical tip from years of data collection: you typically need 20-30 documented episodes before clear functional patterns emerge. It feels like a lot, but patterns become obvious once you have enough data points.
Functional Analysis Considerations
Experimental functional analysis remains the gold standard for identifying behavioral functions, but working with severe aggression requires significant safety modifications.
Safety adaptations might include protective equipment, brief time limits for each condition, multiple trained staff present, clear safety signals for immediate session termination, and controlled environments with minimal risk factors. The science is important, but safety comes first.
Alternative approaches like Interview-Informed Synthesized Contingency Analysis (IISCA) combine suspected maintaining variables into single test conditions. This reduces the number of experimental sessions while maintaining experimental control—a practical compromise for severe cases.
Recent research emphasizes Practical Functional Assessment (PFA) protocols that streamline assessment while maintaining scientific rigor. These approaches acknowledge that traditional functional analysis may not be feasible for all cases of severe aggression, and that's okay.
Building Function-Based Behavior Intervention Plans
Effective behavior intervention plans (BIPs) for aggression integrate multiple components that work together to address why the behavior happens while teaching better alternatives.
Functional Communication Training Strategies
Functional Communication Training (FCT) remains our most empirically supported intervention for aggressive behavior with social functions. The principle is elegant: teach clients to access the same reinforcers they were getting through aggression, but using socially appropriate communication instead.
Communication modality selection depends entirely on the client's current abilities and learning style. Options include vocal communication for emerging speakers, picture exchange or communication apps for visual learners, sign language when motor planning allows, and AAC devices for complex communication needs.
Here's the critical factor many practitioners miss: response effort. The communication response must require less effort than the problem behavior. If aggression involves a simple head-hit, asking the client to navigate through three screens on a communication device won't compete effectively.
Recent research supports Multiple Schedule FCT (mult FCT) approaches that teach clients when reinforcement is and isn't available for functional communication responses. This prevents excessive requesting while maintaining treatment effects—crucial for real-world implementation.
Differential Reinforcement Procedures
Differential Reinforcement of Alternative behavior (DRA) systematically reinforces appropriate behaviors while placing aggression on extinction. Success requires identifying reinforcers of equal or greater value than those maintaining aggression. This sounds simple but requires careful attention to competing reinforcement schedules.
Differential Reinforcement of Other behavior (DRO) provides reinforcement for any behavior except aggression during specified time intervals. This works particularly well when appropriate alternative behaviors are still emerging and you need to create some immediate behavior change.
Differential Reinforcement of Incompatible behavior (DRI) reinforces behaviors physically incompatible with aggression—hands down, appropriate engagement with materials, or specific alternative responses. The beauty of DRI is how it builds replacement behaviors while reducing problem behavior.
Antecedent Intervention Strategies
Modifying environmental conditions reduces the likelihood of aggression while building long-term tolerance and coping skills. This is often where the biggest gains happen.
Environmental arrangement involves reducing triggers through schedule modifications, environmental changes, or task adaptations, while increasing motivation through preferred activities, choice-making opportunities, and appropriate control over the environment.
Proactive teaching strategies include tolerance training that gradually increases exposure to previously triggering conditions, coping skill instruction for self-regulation and communication, and choice-making opportunities that provide appropriate environmental control.
The key insight? Don't just manage triggers—systematically build tolerance to them while teaching better coping strategies.
Crisis and Restrictive Procedures Protocols
When aggressive behavior poses immediate safety risks, you need established protocols that maintain therapeutic relationships while ensuring legal compliance.
Decision Tree for Restrictive Interventions
Level 1: Verbal De-escalation Use calm, supportive tone, provide choices when possible, implement environmental modifications, and offer preferred activities or breaks. Most situations can be resolved at this level if you act early enough.
Level 2: Physical Redirection Guide client to safer location, remove potential hazards, provide additional space from others, and implement predetermined coping strategies. This level requires training and clear protocols.
Level 3: Physical Restraint (Emergency Only) Only when immediate danger exists, trained personnel only, use minimum force necessary, discontinue immediately when safe, and begin crisis debriefing process immediately. This level carries significant legal and ethical responsibilities.
Staff Training Requirements
Anyone working with clients who have histories of aggression needs specialized training that goes beyond basic ABA principles.
Crisis prevention techniques including environmental awareness, trigger recognition, and proactive intervention strategies form the foundation. The best crisis intervention is preventing the crisis.
Safe physical intervention procedures for when restraint becomes necessary, including proper body mechanics, team coordination, and injury prevention. This training requires regular updates and practice.
Post-crisis protocols for ensuring client and staff well-being, conducting immediate safety assessments, and implementing follow-up procedures that strengthen therapeutic relationships.
Legal and ethical considerations surrounding restrictive procedures are becoming increasingly complex. The BACB Ethics Code guidelines provide clear direction, but state regulations vary significantly.
Update: The Joint Commission's 2025 requirements now classify physical holding as restraint, requiring the same documentation and safety protocols as mechanical restraints.
Crisis Data Collection and Debriefing
Immediate documentation following any crisis incident serves multiple purposes—clinical learning, legal protection, and quality improvement.
Include antecedent conditions and triggers, specific behaviors exhibited, interventions attempted and client responses, duration and intensity of episode, any injuries or property damage, and staff involved and their actions.
Crisis debriefing sessions within 24 hours examine alternative interventions that might have prevented escalation, environmental modifications needed, staff performance and learning needs, necessary BIP revisions, and family communication requirements.
These debriefs aren't about blame—they're about learning and improving systems to prevent future crises.
Documentation Standards and Compliance Requirements
Proper documentation serves multiple masters: tracking client progress, ensuring service quality, meeting regulatory requirements, and supporting medical necessity for insurance coverage.
Objective Documentation Principles
Operationally defined behaviors form the foundation of all documentation. Skip the subjective interpretations and focus on what actually happened. "Client engaged in 3 episodes of hitting peers with open hand, each lasting 10-15 seconds, occurring during group activities" provides actionable information.
Frequency, intensity, and duration data offer quantifiable measures of behavior change over time. Track these dimensions consistently using standardized procedures, and your progress reports practically write themselves.
Antecedent and consequent events must be documented to maintain functional validity and guide intervention refinements. This information becomes crucial during treatment reviews and insurance audits.
Incident Summary Requirements
Serious incident reports require comprehensive documentation that tells the complete story while remaining objective and professional.
Include immediate circumstances surrounding the incident, step-by-step description of events from first signs of agitation through resolution, outcome information including any injuries or property damage, and specific follow-up actions implemented.
Recent policy updates from insurance providers effective in 2025 mandate specific documentation elements for ABA services addressing challenging behaviors. Check with your specific payers for their requirements.
PHI Protection and Minimum Necessary Standards
Documentation must balance comprehensive reporting with HIPAA compliance requirements—a tricky balance when dealing with complex behavioral situations.
Minimum necessary principle requires limiting documented information to what's essential for treatment planning, safety, and regulatory compliance. Include what's needed for clinical decisions, but avoid unnecessary personal details about family circumstances or school issues not directly related to behavioral intervention.
Access controls restrict incident reports and sensitive behavioral data to authorized personnel only. Implement role-based access ensuring team members see only information necessary for their specific functions.
Insurance Alignment and Medical Necessity
Documenting medical necessity requires demonstrating that ABA services addressing aggression meet specific criteria established by insurance providers and regulatory bodies. This isn't just paperwork—it's advocacy for your clients.
Capturing Frequency and Intensity Data
Baseline data collection must establish clear metrics that paint a picture of functional impairment before intervention begins. Insurance providers need objective evidence that aggressive behaviors significantly interfere with the client's daily functioning.
Injury risk documentation involves recording instances where aggression resulted in or had potential for physical harm. This information supports the medical necessity argument for intensive behavioral intervention by demonstrating safety concerns.
Functional impairment measures show how aggression affects educational, social, or adaptive functioning. Document specific examples: learning opportunities missed, social relationships affected, community activities restricted due to aggressive behavior.
Progress Monitoring for Payers
Regular data review documenting behavior change over time provides evidence of treatment effectiveness. Insurance providers expect measurable improvement within reasonable timeframes—usually 90 days for initial changes.
Treatment plan adjustments based on data analysis demonstrate clinical responsiveness and continued medical necessity. Document your clinical reasoning for any changes to intervention strategies.
Outcome measures should include both behavioral reduction data and skill acquisition progress. Show how decreased aggression correlates with increased appropriate behaviors and improved quality of life indicators.
Program Review and Quality Assurance
Systematic program evaluation ensures your interventions are actually working while identifying areas needing modification or intensification.
Interobserver Agreement (IOA) Procedures
IOA data collection validates the accuracy and reliability of your behavioral measurements. Collect IOA data for at least 20% of sessions across different observers, settings, and times. This isn't just good practice—it's often required for insurance coverage.
Agreement criteria should meet or exceed 80% agreement for occurrence/non-occurrence measures and 90% for frequency-based measures. Lower agreement indicates need for additional observer training or operational definition refinement.
Treatment Integrity Monitoring
Procedural fidelity ensures interventions are implemented as designed across all team members and settings. Regular integrity checks identify implementation drift and guide staff retraining needs.
Component analysis examines which intervention elements contribute most to behavior change, allowing for streamlined, efficient treatment packages. Why keep implementing procedures that aren't adding value?
Schedule Thinning and Generalization Planning
Systematic reinforcement schedule thinning maintains behavior change while reducing intensive supervision requirements. Document each schedule change and resulting behavioral patterns—this becomes crucial for transition planning.
Generalization programming ensures skills learned in clinical settings transfer to home, school, and community environments. Plan and document generalization activities from day one, not as an afterthought.
Implementation Across Settings
Successful aggressive behavior autism ABA strategies require seamless coordination across all environments where clients spend time, with clear roles for each team member.
Home-Based Implementation
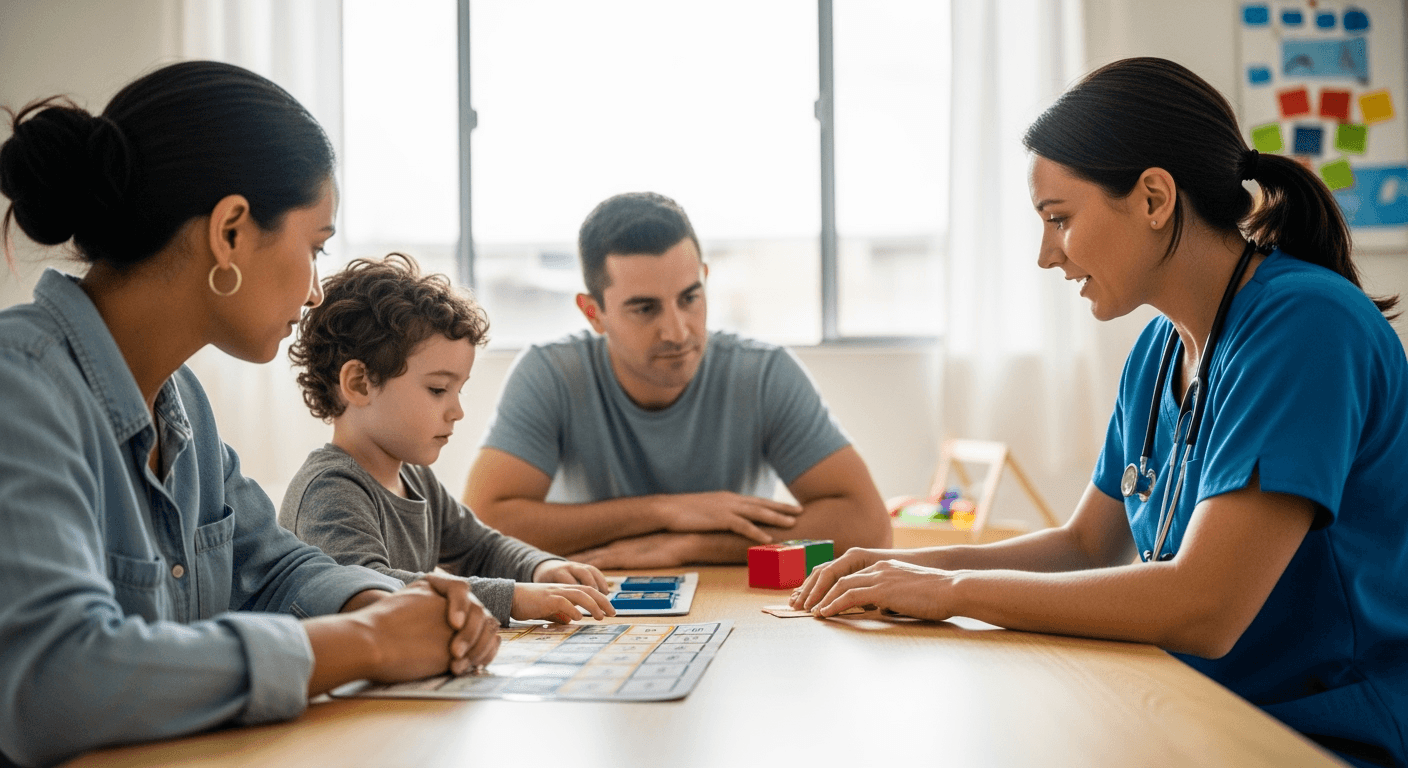
Family training focuses on teaching parents and caregivers to implement intervention procedures consistently. Provide written protocols, hands-on practice opportunities, and ongoing supervision support that respects family routines and values.
Environmental modifications may include removing triggers, creating calm-down spaces, or establishing clear structure that supports appropriate behavior. Work with families to identify practical changes they can maintain long-term.
Crisis planning gives families specific, practiced steps for managing aggressive episodes safely while maintaining intervention integrity. Role-play scenarios and provide written protocols they can reference during stressful moments.
Clinical Setting Considerations
Staff-to-client ratios may need adjustment when working with clients who have histories of severe aggression. Ensure adequate supervision and immediate assistance availability—safety isn't negotiable.
Physical environment modifications include securing potential hazards, creating clear sight lines for supervision, and establishing protected spaces for crisis situations. Think through the space from a safety perspective.
Peer safety protocols protect other clients while maintaining the therapeutic environment. Clear procedures for managing aggression around peers prevent trauma and maintain program integrity for everyone.
School Collaboration
Team coordination requires regular communication between ABA providers, special education staff, general education teachers, and related service providers. Schedule regular team meetings and establish clear communication channels.
Consistency protocols ensure intervention strategies transfer seamlessly between settings while respecting different environmental demands. Document specific procedures for each environment while maintaining functional equivalence.
Crisis response training for school staff ensures safety and intervention consistency when ABA providers aren't present. Provide training that fits within school protocols and legal requirements.
Frequently Asked Questions
What documentation is required when a client engages in aggression during ABA sessions?
Document the incident immediately using objective, observable language. Include specific antecedent conditions, exact behavior topography with frequency and duration, all consequences provided, and any injuries or property damage. Follow your agency's incident reporting procedures and notify supervisors within required timeframes—typically within 24 hours. Remember, this documentation may be reviewed by insurance companies, regulatory bodies, and legal representatives, so accuracy and objectivity are crucial.
How do I determine if functional communication training is appropriate for aggressive behavior?
FCT works best when your functional analysis or assessment data clearly identify social functions (attention, escape, tangible access) maintaining the aggressive behavior. The client must demonstrate some capacity for communication, whether vocal, gestural, or through assistive technology. Consider the response effort required—ensure the communication alternative is more efficient than aggression. If a client can get the same outcome with less effort through appropriate communication, FCT becomes your intervention of choice.
What safety protocols should be in place before implementing interventions for severe aggression?
Establish comprehensive safety protocols including environmental modifications to remove potential hazards, specialized staff training in crisis intervention techniques, clear emergency procedures with designated roles, immediate access to supervisory support, and protective equipment when necessary. All team members must understand restraint procedures and legal limitations before working with clients who have histories of severe aggression. Create written protocols that specify exactly what to do in various crisis scenarios.
How often should behavior intervention plans be reviewed for clients with aggressive behavior?
Review BIPs monthly during the initial implementation phase, with more frequent reviews if data show concerning trends or safety issues. Conduct comprehensive reviews quarterly or whenever significant changes occur in behavior patterns, environmental factors, or client circumstances. Many insurance companies mandate specific review schedules for services addressing challenging behaviors—typically every 90 days for initial authorization periods. Document all reviews thoroughly to demonstrate ongoing clinical oversight.
What constitutes medical necessity for ABA services targeting aggressive behavior?
Medical necessity requires documented evidence that aggressive behavior significantly impairs functional abilities, poses safety risks to self or others, and interferes with learning or social development. Your documentation must include comprehensive baseline data, functional assessment results, evidence that less restrictive interventions have been tried without success, and measurable treatment goals addressing safety and functional improvement. The key is demonstrating that without ABA services, the client faces significant risk of harm or functional decline.
How do new restraint and seclusion regulations affect ABA practice?
The Joint Commission's 2025 updates classify physical holding as restraint, requiring the same documentation and safety protocols as mechanical restraints. This means any physical intervention restricting movement must be treated as restraint with proper training, immediate documentation, and post-incident debriefing. Review your state regulations for additional requirements—some states have more restrictive guidelines than federal standards. The trend is clearly toward greater oversight and documentation requirements for any restrictive procedure.
Conclusion
Managing autism aggression ABA interventions successfully requires clinical expertise, unwavering attention to safety, and meticulous documentation practices that serve multiple stakeholders. But here's what I've learned after years in this field: when we get it right, the impact extends far beyond just reducing problem behavior.
Effective aggression intervention transforms lives. Clients learn to communicate their needs appropriately, families regain confidence in managing challenging situations, and communities become more accessible. The work is difficult, demanding, and sometimes heartbreaking—but it's also deeply meaningful.
The regulatory landscape continues evolving, with updated restraint protocols and enhanced documentation requirements from insurance providers. Stay informed about these changes while maintaining your focus on what matters most: client safety, progress, and quality of life.
Success in this area requires ongoing professional development, consultation with experienced colleagues, and regular engagement with emerging research. The complex challenges of aggression intervention demand our most thoughtful, evidence-based, and compassionate clinical practice.
Remember: every crisis prevented, every communication skill taught, and every family supported represents progress toward a more inclusive world for individuals with autism. That's work worth doing well.
Popular in Behavior Analysis Concepts
- 1
ABA Graph Analysis Terms: Level, Trend, Variability
2,6736 min read - 2
Partial Interval vs Whole Interval vs MTS: ABA Guide
2,4136 min read - 3
Master IOA Formulas and Methods for Data Integrity
2,0148 min read - 4
ABA Prompting Hierarchy & Prompt Fading: RBT How-To Guide with Examples
1,4017 min read - 5
Functional Behavior Assessment ABA: Complete 2025 Guide [Step-by-Step]
1,2056 min read
Popular in Behavior Analysis Concepts
- 1
ABA Graph Analysis Terms: Level, Trend, Variability
2,6736 min read - 2
Partial Interval vs Whole Interval vs MTS: ABA Guide
2,4136 min read - 3
Master IOA Formulas and Methods for Data Integrity
2,0148 min read - 4
ABA Prompting Hierarchy & Prompt Fading: RBT How-To Guide with Examples
1,4017 min read - 5
Functional Behavior Assessment ABA: Complete 2025 Guide [Step-by-Step]
1,2056 min read
Related Resources
Explore more helpful content on similar topics
![Maladaptive Behavior ABA: The Complete Guide for RBTs & BCBAs [2025] Illustration showing a person at a symbolic crossroads, with abstract shapes hinting at different behavioral paths.](/_next/image?url=https%3A%2F%2Fl0qdfezqmw69fxn5.public.blob.vercel-storage.com%2Fresources%2Fmaladaptive-behavior-aba-strategies-1756045621241.png&w=3840&q=75)
Maladaptive Behavior ABA: The Complete Guide for RBTs & BCBAs [2025]
Learn how to document and reduce maladaptive behavior ABA effectively with evidence-based strategies and clear session note guidelines for better outcomes.
Autism Aggression Family Guide: Working with ABA Teams
Learn effective home strategies and ABA tips in this autism aggression family guide to support your child and create a safer, calmer environment.
Prompt Dependency in ABA: Signs & Fading Guide
Discover prompt dependency in ABA: spot signs like waiting for prompts and over-reliance. Learn simple fading techniques to build client independence. Essential guide for beginner RBTs and parents.