Essential Guide to CPT 97155 Unbundled Authorization
Introduction to the CPT 97155 Documentation Shift
Steering through ABA billing changes can be tough for BCBAs these days, especially with recent shifts emphasizing granular oversight. As payers tighten requirements, the move toward CPT 97155 unbundled authorization demands precise documentation to justify protocol modifications and ensure reimbursement. This update is particularly critical for practices serving clients under Medicaid or commercial plans, where bundled approvals are phasing out in favor of code-specific requests. By mastering these changes, you can safeguard your workflow, minimize audit risks, and maintain uninterrupted care.
In this article, you'll discover the documentation shift for CPT 97155, its workflow impacts, detailed requirements for justifying decisions, separation from 97153, tips for authorization requests, and audit preparation using a Virginia Medicaid example. These insights draw from authoritative guidelines to empower your practice.
Here are 3-5 key takeaways to guide you:
- Unbundled authorizations require separate requests for CPT 97155, focusing on protocol modifications by qualified health professionals.
- Documentation must tie changes to client data, including rationale, outcomes, and session details for billing accuracy.
- Expect more frequent renewals and audits, but proactive prep can reduce denials and support evidence-based ABA.
- Distinguish 97155 from 97153 by tracking QHP involvement versus technician delivery.
- Use payer-specific guidelines, like Virginia Medicaid's, to align notes and authorizations.
ABA providers have long relied on comprehensive documentation to demonstrate medical necessity, but recent updates for CPT 97155—adaptive behavior treatment with protocol modification—signal a more rigorous standard. Effective in late 2024 and intensifying into 2025, payers are requiring unbundled authorizations that isolate this code from broader ABA services. According to the ABA Coding Coalition (2024), QHP protocol modifications apply only when a qualified health professional (QHP) like a BCBA is directly engaged with the patient or directing a technician while modifying protocols. This shift stems from efforts to enhance billing precision and accountability, reducing overgeneralized approvals that previously bundled 97155 with direct treatment codes.
For BCBAs, this means shifting from high-level progress reports to session-specific notes that capture real-time adjustments. The change aligns with broader telehealth expansions, where modifiers like 95 or GT must accompany 97155 for remote delivery. Practitioners report that while initial adaptation requires effort, it ultimately supports better clinical outcomes by tying modifications directly to client data as shown in hybrid ABA models.
Breakdown of CPT 97155 Unbundled Authorization and Its Impact on BCBA Workflow
Unbundling CPT 97155 requires separate service authorizations for this code, decoupling it from overarching ABA plans. Starting October 15, 2025, in programs like Virginia Medicaid, providers can no longer submit a single request encompassing all services under 97155; instead, authorizations must specify units for protocol modifications. This stems from payer directives to prevent fragmented billing and ensure each code reflects distinct clinical activities, as outlined in the Virginia Medicaid guidelines.
The impact on BCBA workflows is varied. First, it necessitates more frequent authorization renewals, potentially monthly, to align with 97155's requirement for at least one direct supervisory session per month. You must now allocate time for code-specific justifications, integrating protocol modification documentation into daily notes. This can streamline long-term planning by highlighting modification efficacy but may initially increase your administrative load with more prep time.
To adapt, consider ABA billing precision tools like session note templates that auto-flag modification sections. You'll find this ensures compliance while preserving focus on client progress. Over time, it fosters a more evidence-driven practice, helping you balance paperwork with hands-on care.
Detailed Documentation Requirements for CPT 97155 Unbundled Authorization: Justifying Clinical Decision-Making, Protocol Modifications, and Client Response
Effective documentation for CPT 97155 must substantiate the QHP's direct involvement and the necessity of modifications. Key elements include recording all protocol changes, such as target adjustments or intervention tweaks, with rationale tied to client data. The TRICARE guidelines emphasize noting observations on goal progress, barriers encountered, and client responses during the session.
For justifying clinical decision-making, include objective measures like pre- and post-intervention data, such as frequency of targeted behaviors before and after a fade procedure. Protocol modification documentation should detail what was changed—e.g., increasing reinforcement density for skill acquisition—and why, linking it to evidence of stagnation or regression. Client response notes must capture behavioral indicators, like increased engagement or reduced maladaptive actions, to demonstrate ongoing medical necessity.
You can structure notes around these core components to keep things clear. Start with session identifiers: date, duration, and participants (QHP, client, technician if applicable). Then cover modifications applied, such as "Adjusted token economy from 1:5 to 1:3 ratio based on 20% error rate in data." Finally, add rationale and outcomes: clinical justification supported by graphed progress, plus immediate client feedback.
This level of detail not only supports billing but also informs future sessions. It boosts ABA billing precision and helps you track what works best for each client.
Guidance on Separating 97155 (Protocol Mod) from 97153 (Direct Treatment)
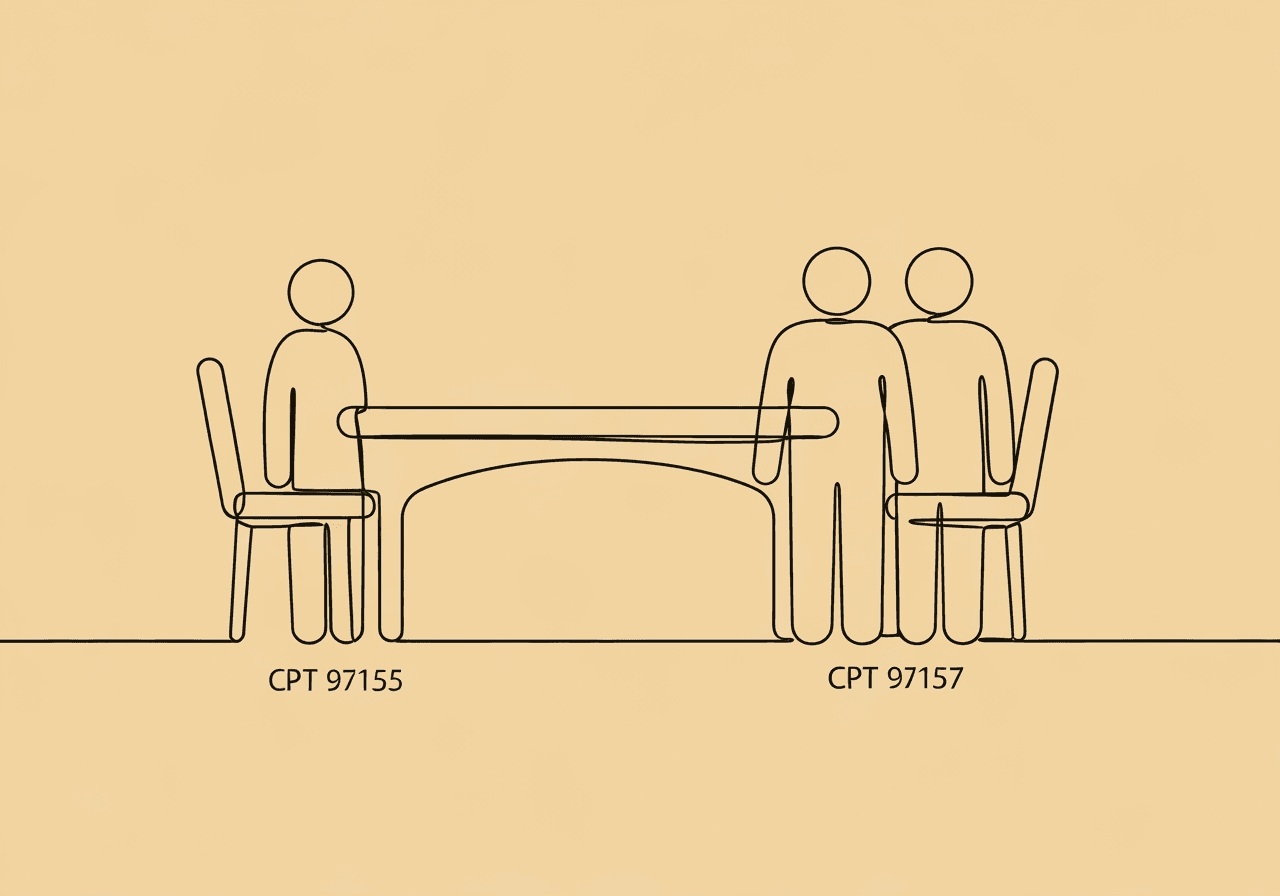
Distinguishing CPT 97155 from 97153 is essential to avoid claim denials, as each targets different provider roles. CPT 97153 covers adaptive behavior treatment by protocol delivered by a technician (e.g., RBT) under QHP direction, focusing on direct, face-to-face implementation without modifications. In contrast, 97155 requires the QHP's active participation in protocol adjustments, supervision, or direct treatment, as per the ABA Coding FAQs.
Concurrent billing is permissible in many payers when the QHP directs the technician while modifying protocols, but separation hinges on activity logs. For instance, bill 97153 for the technician's uninterrupted delivery of scripted interventions, while allocating 97155 time to the BCBA's concurrent troubleshooting or plan updates. The Virginia Medicaid FAQs allow joint billing for supervision but prohibit overlap in non-distinct activities, such as passive observation.
To separate effectively, time-track distinct contributions—e.g., 30 minutes of 97153 for RBT-led drills, 15 minutes of 97155 for BCBA-led fading. Document QHP presence and role explicitly to justify 97155. Use modifiers for telehealth if the QHP joins remotely.
This delineation promotes ABA billing precision and reduces audit scrutiny. You'll avoid common pitfalls by keeping records straightforward and tied to actual activities.
Strategic Tips for CPT 97155 Unbundled Authorization Requests
Crafting authorization requests for CPT 97155 unbundled authorization involves projecting units based on clinical needs while anticipating payer scrutiny. Start by estimating monthly sessions—typically one minimum per client—supported by historical data showing modification frequency. Include projected outcomes, like "10 units to address plateaued social skills via protocol tweaks," tied to assessment results.
Tailor requests to payer guidelines; for example, specify face-to-face requirements and exclude indirect planning time. The ABA CPT guide recommends bundling rationale with progress summaries from recent notes to demonstrate necessity.
Practical strategies can make this smoother. Run pre-submission checklists to verify unit breakdowns match planned interventions, avoiding overestimation. Integrate evidence by attaching graphed data that shows why modifications are warranted—this can boost approval odds. Time renewals for 30 days pre-expiration, incorporating interim progress to extend seamlessly.
These steps ensure requests align with unbundled standards. They minimize disruptions and keep your practice running smoothly.
Preparing for Audits Under New CPT 97155 Unbundled Authorization Standards (Including Virginia Medicaid Example)
Audits for CPT 97155 focus on verifying medical necessity, accurate unit billing, and QHP involvement amid unbundled authorizations. Payers review contemporaneous notes for modification details, progress linkages, and supervision compliance, often requesting records within 30 days as outlined in Medicaid audit protocols. In Virginia Medicaid, effective October 2025, audits emphasize service authorization forms specifying 97155 units, with monthly LBA/LABA/LMHP observations required. The DMAS manual mandates retaining ISPs, assessments, and notes on-site for potential reviews, targeting fraud detection through credential and time verifications.
Preparation starts with audit-ready files organized by client, including indexed sections for authorizations, notes, and data. Avoid common pitfalls by ensuring notes differentiate 97155 activities—vague entries often trigger denials. For Virginia-specific needs, use the new form for post-October 2025 starts, documenting annual assessments and family involvement.
By proactively aligning documentation, you can navigate audits confidently. This preserves reimbursement integrity and lets you focus on client care.
Frequently Asked Questions
What are the specific documentation requirements for CPT code 97155 in 2025?
Documentation must include all protocol modifications, rationale, client responses, and objective data like progress toward goals. The QHP must be directly involved face-to-face or via telehealth, with notes detailing barriers and session participants. According to TRICARE guidelines (2024), note protocol changes. Monthly minimum sessions apply, supporting medical necessity.
How does the unbundling of CPT code 97155 affect billing and reimbursement?
Unbundling requires separate authorizations per code, ending bundled ABA requests and mandating unit-specific justifications starting October 2025 in states like Virginia. This promotes precise billing but may delay approvals if documentation lacks detail. The ABA Coding Coalition (2024) notes distinct QHP reimbursement, potentially increasing scrutiny but improving long-term funding accuracy.
What are the differences between CPT codes 97153 and 97155?
97153 bills for technician-delivered protocol treatment, while 97155 covers QHP-led modifications or supervision. Concurrent billing is allowed when distinct, but some payers like North Carolina Medicaid prohibit it for overlapping care. Per Virginia Medicaid FAQs (2025), 97155 needs direct QHP engagement, emphasizing adjustments over routine delivery.
How often should CPT code 97155 be reported for monthly authorization?
Report 97155 at least monthly for one supervisory/modification session per client, with additional units as clinically needed. Authorizations must specify projected units; assessments like 97151 do not require prior approval. Virginia Medicaid (2025) guidelines align with provider observations.
Are there new telehealth modifiers required for CPT code 97155 in 2025?
Yes, use modifier 95 or GT for remote 97155 sessions to indicate telehealth delivery while ensuring face-to-face equivalents. The S Cubed guide (2025) confirms telehealth code pairing, subject to payer rules excluding indirect activities.
What are the audit requirements for Virginia Medicaid ABA services under 97155?
Audits verify unit accuracy, QHP credentials, and documentation matching billed services, requiring on-site retention of notes and ISPs. Monthly observations and annual assessments are mandatory. DMAS (2024) stresses fraud prevention compliance, with availability on request.
As CPT 97155 unbundled authorization takes hold post-fall 2025, BCBAs must prioritize protocol modification documentation to uphold ABA billing precision and compliance. This shift, while demanding, reinforces evidence-based practice by linking adjustments to measurable client outcomes as supported by parent-led ABA studies, drawing from payer guidelines like the ABA Coding Coalition and Virginia Medicaid.
Key implications include reduced bundled efficiencies but heightened accountability. Proactive preparation may help lower denial rates. To implement effectively, audit your current notes against requirements, train teams on separations from 97153, and integrate tools for seamless authorizations. Start by reviewing one client's file this week—update templates for modification rationale and project units for renewals. Ultimately, these practices ensure continuity of care, empowering you to deliver impactful ABA services without reimbursement hurdles.
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,4048 min read - 2
CPT Code 97153: Complete Guide for RBTs
3,8699 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
2,8479 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,4044 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,6457 min read
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,4048 min read - 2
CPT Code 97153: Complete Guide for RBTs
3,8699 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
2,8479 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,4044 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,6457 min read
Related Resources
Explore more helpful content on similar topics
CPT 97155 Documentation Narrative: A BCBA Guide
Master CPT 97155 documentation narratives for BCBA protocol modifications. Get step-by-step guidance on data-driven justifications, billing compliance, and ABA therapy standards to ensure accurate reimbursements.
CPT 97155 vs 97157: Documentation Guide for BCBAs
Master CPT 97155 vs 97157 documentation for BCBAs. Discover key differences in service definitions, required elements, ethical tips, and scenarios for group adaptive behavior treatment and protocol modifications to ensure compliance.
CPT 97155 No Protocol Mod: BCBA Documentation Guide
Learn how to navigate CPT 97155 no protocol modification for BCBA supervision billing. Discover key differences in 97155 vs 97157 documentation, essential tips for compliance, and strategies to avoid billing audits.