CPT 97155 vs 97157: Documentation Guide for BCBAs
CPT 97155 vs 97157: Documentation Guide for BCBAs
Getting a handle on CPT 97155 vs CPT 97157 documentation can be tough for BCBAs, particularly with payers watching billing closely. Incorrect coding or incomplete notes not only risks claim denials but can also lead to ethical lapses in service delivery. According to the ABA Coding Coalition, precise documentation ensures compliance while focusing on client-centered care.
This guide breaks down the core differences between these codes, helping you document effectively to support medical necessity and treatment fidelity. You'll learn the service definitions, including who qualifies as the "client" (the patient for 97155 versus multiple caregivers for 97157), detailed documentation requirements for each, ethical considerations, and real-world scenarios. By the end, you'll have a summary table and actionable steps to choose the right code every time. For more on ABA basics, check out our ABA coding fundamentals guide.
Core Distinctions Between CPT 97155 and CPT 97157
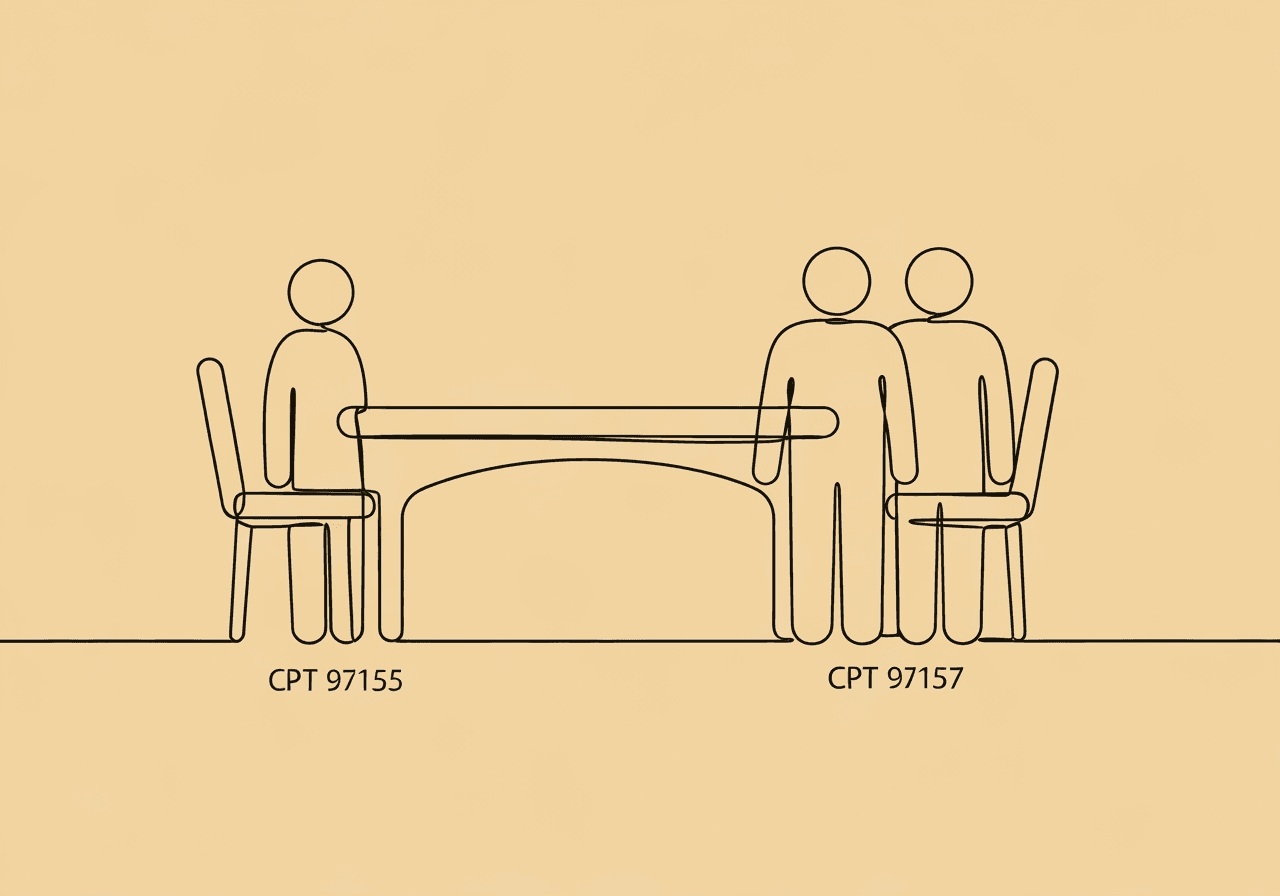
CPT codes 97155 and 97157 both fall under adaptive behavior treatment in ABA, but they serve distinct purposes in protocol modification and caregiver guidance. According to the American Academy of Professional Coders (AAPC) (2024), CPT 97155 focuses on direct, individualized adjustments to a client's treatment plan, while CPT 97157 emphasizes group-based training for families.
The primary difference lies in the service focus and participants. For CPT 97155, the "client" is the patient, requiring face-to-face interaction where the BCBA observes and modifies protocols in real time. This code cannot apply to group sessions or caregiver-only training. In contrast, CPT 97157 treats multiple caregivers as the clients, delivered without the patient present, to build their skills in managing behaviors at home.
Both codes bill in 15-minute units and require a qualified health professional (QHP), such as a BCBA, to deliver the service. However, 97155 demands active clinical decision-making tied to the patient's response, whereas 97157 prioritizes interactive group dynamics and skill transfer to daily routines.
Understanding these distinctions prevents common pitfalls like misbilling indirect activities under 97155, which the ABA Coding Coalition clarifies as non-billable.
Service Definitions: Who Is the Client and What Happens in Each Session?
In CPT 97155, the service is adaptive behavior treatment with protocol modification, administered face-to-face by a BCBA or other QHP with one patient. The ABA Coding Coalition (2024) specifies that the BCBA must directly engage with the patient or simultaneously direct a technician while implementing modifications. This includes observing behaviors, analyzing data, and adjusting interventions on the spot—for instance, fading prompts if the client masters a skill ahead of schedule.
The client here is unequivocally the patient, ensuring the session addresses their adaptive needs. Caregivers may participate, but the focus remains on the patient's progress. Sessions can occur in clinics, homes, or via telehealth (per AMA guidelines), but the BCBA's presence is mandatory for billing.
Shifting to CPT 97157, this code covers multiple-family group adaptive behavior treatment guidance, also face-to-face by a QHP, but without the patient present. AAPC guidelines (2024) define it as training at least two sets of guardians or caregivers (up to six units per day) on techniques to reduce maladaptive behaviors and build skills. The "client" is the group of caregivers, with the goal of empowering them to reinforce therapy outside sessions.
Topics might include behavior identification, reinforcement strategies, or crisis management, tailored to each family's treatment plan. Unlike 97155, no direct patient interaction occurs, and groups must involve multiple families to qualify—individual family training uses CPT 97156 instead.
These definitions highlight a key compliance note: Mixing patient presence with group caregiver training could invalidate billing for either code, as confirmed by the ABA Coding Coalition.
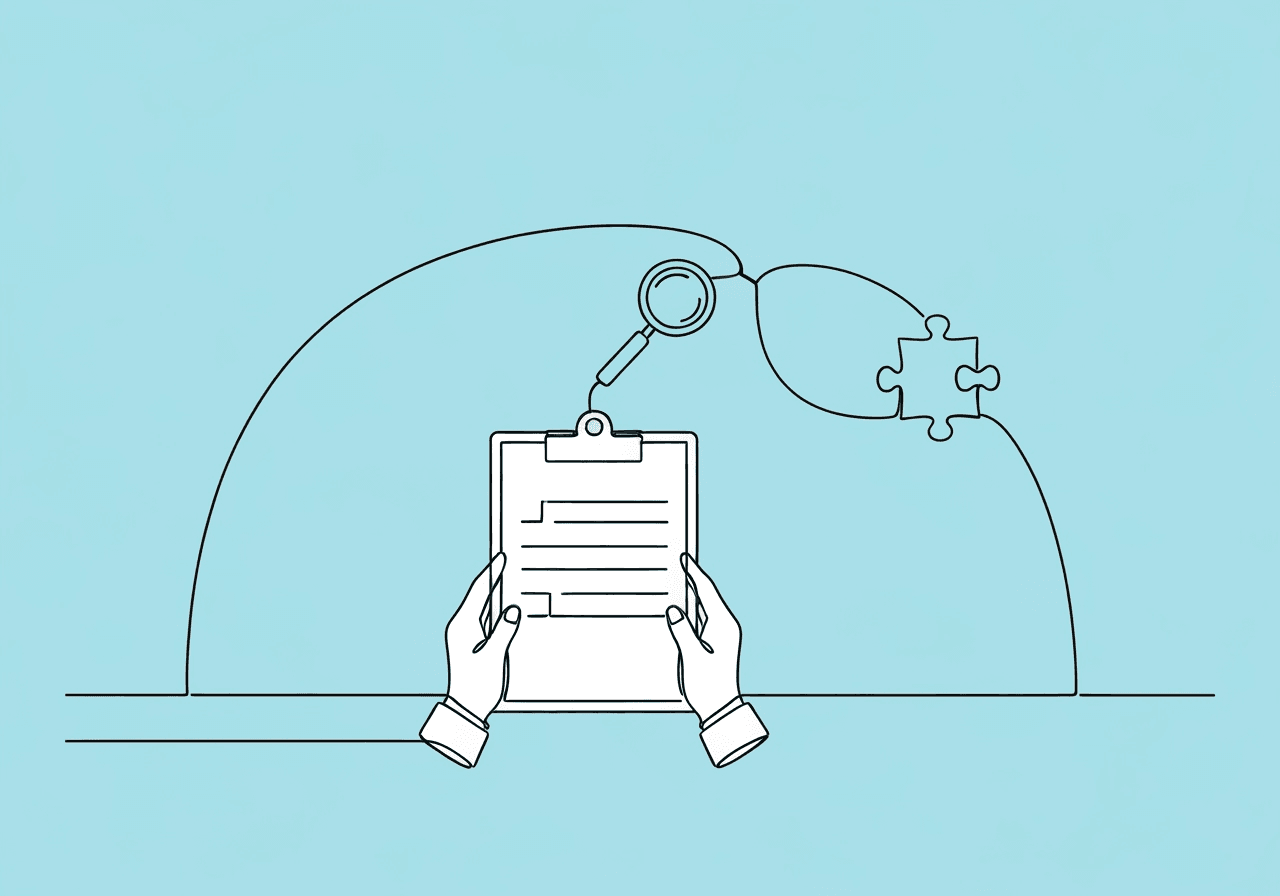
Required Documentation for CPT 97155: Capturing Protocol Modifications
Thorough protocol modification documentation for CPT 97155 proves the BCBA's active role in real-time adjustments, justifying medical necessity. Start with session logistics: Record exact start and stop times, total units billed, location, and all attendees, including any technicians directed. Brellium's ABA guide (2024) emphasizes objective language, such as "BCBA observed client's latency to comply at 45 seconds and modified prompt hierarchy from full to partial."
Key elements include:
- Direct client data: Quantify behaviors observed, like success rates or error patterns. Use graphed probes or session logs for this.
- Justification for protocol changes: Explain the clinical rationale—e.g., "Reduced trials from 10 to 6 due to 90% mastery criterion met, per ABC data analysis." Link it clearly to evidence.
- BCBA presence and actions: Detail face-to-face involvement, such as modeling skills for the patient or coaching a technician mid-session. Include timestamps where possible.
- Patient response: Note immediate outcomes, like improved engagement, to link modifications to progress.
Avoid vague phrases like "client did well"; instead, tie everything to the individualized treatment plan (ITP). Payers often require structured notes like SOAP (Subjective, Objective, Assessment, Plan) to audit these details, though format may vary. If no modifications occur, do not bill 97155—revert to supervision codes like 97153, as outlined in ABA Coding Coalition FAQs.
Consistent use of templates, such as those from Praxis Notes, simplifies this process while ensuring HIPAA compliance. See our ABA documentation templates resource for examples.
Required Documentation for CPT 97157: Emphasizing Group Dynamics and Caregiver Engagement
For CPT 97157, documentation shifts to the collective experience of caregivers, demonstrating how group training advances each patient's ITP. Begin with attendance: List names, relationships to patients, and contact info for at least two families, along with session date, duration, and topics covered. Humana's ABA policy (2024) requires noting the QHP's role and any support staff.
Essential components are:
- Group dynamics: Describe interactions, such as "Caregivers role-played differential reinforcement, sharing home examples from their child's challenging behaviors." Highlight key exchanges.
- Topics covered: Outline behavioral techniques taught, like token economies or functional communication training. Reference handouts or agendas used.
- Caregiver participation: Quantify involvement—e.g., "All five participants practiced scripting responses, with 80% reporting intent to implement at home." Note any standout contributions.
- Link to treatment plan: Connect content to specific patient goals, such as "Session reinforced chaining for Client A's self-care skills, aligning with ITP objective 2.3."
Since patients are absent, emphasize skill generalization to home settings. Reauthorization may need evidence of at least six sessions every six months, per some payers. Use structured formats like DAP (Data, Assessment, Plan) to capture group-specific insights without patient data.
This approach not only supports billing but also highlights the code's value in scalable family support.
Ethical Considerations in Using CPT 97155 vs CPT 97157
Ethical use of these codes aligns with the Behavior Analyst Certification Board (BACB) Ethics Code for Behavior Analysts, prioritizing client welfare and integrity. For CPT 97155, the principle of "do no harm" (BACB Code 2.09) requires modifications to be evidence-based, avoiding unnecessary changes that could disrupt progress. Advanced Autism Services (2024) stresses obtaining informed consent for real-time adjustments, ensuring families understand risks like temporary behavior extinction bursts.
Billing ethics are critical: Bill 97155 only for documented protocol work, not passive observation or planning—upcoding here violates BACB 1.04 on Integrity. In group vs. individual delivery, select 97157 ethically when it promotes generalization without diluting individualized care; larger groups (beyond clinical justification) may compromise fidelity.
For CPT 97157, maintain confidentiality across families (BACB 2.06), using anonymized examples in discussions. Transparency is key—disclose group formats upfront to avoid misleading families about one-on-one attention. Financial pressures, like maximizing units, should never override competence (BACB 1.05); for instance, do not inflate attendance to meet minimums. For full details, review the BACB Ethics Code.
Overall, both codes demand accurate representation in notes to prevent fraud, fostering trust with payers and families. Consult BACB resources for ongoing guidance. Our ABA ethics overview covers more on daily application.
Practical Scenarios: Deciding Between CPT 97155 and CPT 97157
BCBAs often face decisions on coding during busy caseloads. Consider a session where a BCBA joins an RBT mid-therapy to address a client's emerging elopement: Observe, probe safety responses, and modify the escape extinction protocol on-site. Bill as CPT 97155, documenting the adjustment and patient's calmer transitions. This scenario fits because the patient is present, and changes are direct.
Now imagine training three families on handling mealtime refusals: Without patients there, facilitate discussions on noncontingent access and data tracking, linking to each ITP. Use CPT 97157, noting participation levels and home application plans. If only one family attends, switch to 97156 to maintain compliance.
In hybrid cases, like a BCBA modifying a plan while caregivers watch, prioritize 97155 for patient focus—separate caregiver debriefs could qualify as 97157 if grouped. Always review payer policies; for example, telehealth expansions allow both codes remotely, but documentation must confirm face-to-face equivalents, as detailed in ABA Coding Coalition telehealth guidance.
These examples underscore auditing sessions post-hoc to align coding with BACB ethics and AMA definitions. For more on pitfalls, visit our billing errors checklist.
Summary Table of Key Differences
| Aspect | CPT 97155 | CPT 97157 |
|---|---|---|
| Service Focus | Protocol modification and direct treatment | Group caregiver guidance and skill training |
| Client Present? | Yes (patient is the client) | No (multiple caregivers are clients) |
| Billing Units | 15 minutes, face-to-face with patient | 15 minutes, up to 6 units/day per group |
| Documentation Focus | Real-time changes, patient data, BCBA actions | Group topics, participation, ITP links |
| Common Scenario | Adjusting interventions during therapy | Training families on behavior management |
| Ethical Note | Justify modifications to avoid upcoding | Ensure confidentiality in group settings |
This table, drawn from ABA Coding Coalition guidelines (2024), aids quick reference for compliance.
Frequently Asked Questions
What are the specific documentation requirements for CPT 97155?
Documentation for CPT 97155 must include start/stop times, BCBA's face-to-face presence, detailed protocol modifications with clinical rationale, patient responses via objective data, and any technician direction. Brellium (2024) recommends quantifiable notes, like success percentages, to prove medical necessity and avoid denials.
How does CPT 97157 differ from CPT 97156 in terms of documentation?
CPT 97157 requires group-specific details like multiple family attendance and interactive dynamics, while 97156 focuses on one family's individualized guidance. Both link to the ITP, but 97157 emphasizes collective participation without patients present, per AAPC (2024). Payers may audit for minimum group sizes.
What are common mistakes in CPT 97155 vs CPT 97157 documentation?
Frequent errors include billing 97155 without actual modifications or including patient data in 97157 notes. ABA Coding Coalition (2024) warns against vague language; always specify attendee roles and tie content to plans to prevent audits.
Can CPT 97155 include caregiver training, and how does that impact billing?
Caregivers can observe in 97155, but training alone does not qualify—focus remains on patient modifications. If training dominates, use 97157 for groups. Humana policy (2024) requires separating services to ensure ethical, accurate billing.
How do payers enforce compliance for these codes?
Payers review for medical necessity via detailed notes; for 97155, expect scrutiny on modification evidence, while 97157 needs attendance proofs. Telehealth allowances vary, but AMA guidelines (2024) mandate equivalent documentation standards.
When should a BCBA choose group adaptive behavior treatment under CPT 97157?
Opt for 97157 when training multiple families enhances efficiency and generalization, like shared strategy sessions. Ensure at least two families and no patient involvement, as outlined by Ensora Health (2024). Document rationale to align with ITP goals.
Wrapping up, mastering CPT 97155 vs CPT 97157 documentation empowers BCBAs to deliver compliant, impactful ABA services. By distinguishing direct patient modifications from group caregiver guidance, you uphold ethical standards and minimize billing risks, ultimately benefiting client outcomes.
To apply this knowledge, audit your next session notes against the requirements outlined. Develop a checklist for protocol changes in 97155 and group metrics in 97157. Finally, consult your payer's policy manual or a compliance expert for case-specific nuances—staying proactive ensures sustainable practice.
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,6858 min read - 2
CPT Code 97153: Complete Guide for RBTs
4,0939 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
3,0829 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,5454 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,7627 min read
Popular in CPT Codes & Billing
- 1
2025 ABA Billing Updates: Essential Guide for RBTs
5,6858 min read - 2
CPT Code 97153: Complete Guide for RBTs
4,0939 min read - 3
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
3,0829 min read - 4
CPT Code 97153 ABA: Complete 2025 Billing Guide for RBTs & BCBAs
2,5454 min read - 5
BCBA Initial Authorization Checklist: Simplify ABA Approvals
1,7627 min read
Related Resources
Explore more helpful content on similar topics
CPT 97155 vs 97156 Documentation: Key Differences for BCBAs
Unravel CPT 97155 vs 97156 documentation differences for BCBAs. Learn essential breakdowns, side-by-side comparisons, ABA billing compliance tips, and real-world scenarios to master accurate coding and avoid compliance risks.
Master ABA CPT Codes 97153-97158: Avoid Costly Audit Findings in 2025
Learn how to navigate ABA therapy CPT codes 97153–97158 for compliant billing, audit-proof documentation, and maximizing 2025 ABA insurance reimbursements.
CPT 97155 Documentation Guide for BCBAs: Audit Compliance
Master CPT 97155 documentation for BCBAs: Essential guide to protocol modification, client responses, and audit-proof workflows. Learn to avoid red flags and ensure full compliance in ABA billing.